Sometimes it fails, but it's remarkable how often it works.
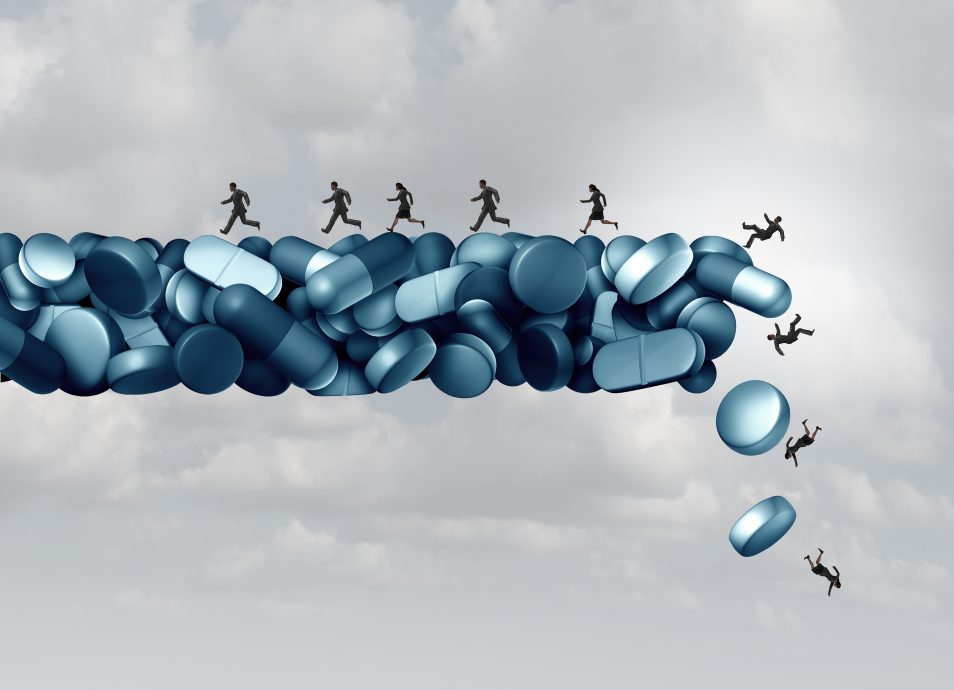
Don't Make Anti-Opioid Laws the Villain Here
Advocacy of legalized narcotics is not new, but Jeffrey Miron’s recent formulation, “Legalizing Opioids Would Dramatically Reduce Overdoses,” combines ignorance and skewed accounting.
When assessing the damage associated with the use of powerful narcotics, Miron looks to restrictions on availability as the real cause of adverse outcomes, attributing negative effects to the presence of the controls, while offering an inadequate accounting of the damage from continued, and unrestricted, use of the substances themselves.
This argument requires an inversion of logic. Confronting a litany of harms from the use of a dangerous substance, he finds the fault not in ourselves, nor the substance, but rather in our laws. To Miron, it is the restrictions levied on the substances that are the greater “cause” of damage.
One almost hears an echo of Jean-Jacques Rousseau regarding the evils of societal constraints on natural man, though in this case it is the libertarian “market” that acquires a tinge of nobility.
In a short space I cannot respond to all the errors in Miron’s essay (which he wrote in response to Robert VerBruggen’s Liberty Forum piece this month), but I can make a case against the central thrust of his argument, namely the claim that “prohibition,” or efforts to restrain, regulate, monitor, supervise, or legally deny substances that can kill, should be deemed an all-purpose villain that only makes matters worse.
Conversely, of course, limitless availability and use of the same substances, by the logic Miron offers, presents few dangers, and—even less plausibly, as it seems to me—will somehow lower the overall risk of addiction’s consequences to the individual and society. Hence, Miron argues, when it comes to opioids, greater availability and use should be pursued as ameliorative public policy.
To arrive at this conclusion Miron overlooks (or miscalculates) known facts about opioid dependence on the individual, as well as the realistic social, public health, and criminal justice consequences of unfettered drug availability.
For example, consider the problem of the addict’s ever-increasing tolerance of opiods, a physiological response that is inherent in their use. Tolerance of course requires escalating dosages to achieve the same effect, increasing thereby the risk of overdose. But not after the logical inversion that Miron proposes. The real problem, says he, stems from our efforts to restrict escalating doses. Miron writes that “prohibition further increases overdoses by disrupting tolerance, which makes use less dangerous as the body develops resistance to opioids’ respiratory-depressing effects.”
Whatever is meant by “disrupting tolerance,” this statement does not evince a medically sound view of tolerance. A real problem of escalating opioid use is that of “differential tolerance” by different bodily systems in response to opioid exposure. Analgesic tolerance appears quickly, but the threat of respiratory depression is still present nonetheless, because the rate of tolerance to opioid exposure in the respiratory system progresses less rapidly. Users who seek either pain relief or euphoria increase dosages in a manner that escalates their risk of fatal consequences.
Were the use of opioids to expand in an unrestricted manner, there is no doubt that the toll of overdose deaths, driven by increased prevalence of use, and increased lethality of the substances available on the “market” at the escalating dosages desired, would rise to staggering levels.
We are told further that escalating opioid use does not produce organ damage and that there is “no dosage ceiling” for their analgesic effect, hence the conclusion that limitations on dosages “make little sense.”
Again, these claims are not accurate. Miron does not take into account the real risk of increased sensitization to pain experienced by those escalating opioid doses, in the phenomenon known as “hyperalgesia,” which is the perverse effect of experiencing even greater pain through chronic high-dose exposure.
What the user experiences is a double trap: Increased dosage leads to sensitized experience of pain and diminished euphoria, which can be met only by stepping up use, which raises the likelihood of death by overdose. This biological effect is not a function of “prohibition.” Rather, the more drug that is used, the greater the danger. Moreover, the brain, the neurophysiology of which is transformed by addiction, is clearly an organ, and the impact does indeed seem to amount to organ damage.
Consider also that the great majority of those who overdose on opioids are concurrent users of other substances, licit and illicit.
Data collected in Florida by the Florida Drug-Related Outcomes Surveillance and Tracking System (FROST, which does toxicological testing on all drug overdose cases in the state) found that about 95 percent of opioid overdoses involve other drugs—on average, two to four others, and even up to 11 others.
Theodore J. Cicero, Matthew S. Ellis, and Zachary A. Kasper published the results of their recent study of nearly 4,500 individuals undergoing treatment for opioid addiction in the February 2017 edition of the journal Addictive Behaviors. They found that marijuana was used by 87 percent of those being treated, and alcohol by 93 percent, while benzodiazepines were very common adjuncts to opioid abuse and especially overdose. The authors’ conclusion was that “physicians should routinely ascertain complete licit and illicit drug histories in patients for whom they prescribe opioids.”
Clearly many of those at risk from opioid use, whether prescription-sourced or from the illicit drug market, are already regular abusers of multiple substances which they have little difficulty finding in sufficient quantity. If anything, one would think that greater restrictions on multiple substance abuse and the initiation thereof would be effective counters.
Miron is well aware of this pattern of multi-drug consumption and overdose risk, but for him, once again, the problem is our efforts at regulation and control through law. As he writes:
Prohibition . . . makes opioids more dangerous by encouraging drug mixing. . . . If opioids are easily accessible, people tend to use the substance they desire; when access is limited, however, some consumers obtain an insufficient quantity and therefore improvise with alcohol, benzodiazepines, and other drugs.
This gets it backwards. There is a clear progression in risk behavior, with substance abusers adding more drugs in combination, to which they then add potentially lethal opioids. How could allowing “consumers” to obtain a limitless quantity of opioids inhibit them from using, either initially or concurrently, alcohol, marijuana, or sedatives?
We should acknowledge that it is the use of the drugs themselves, and not efforts at protection, that produce the greater risk.
Now for the question of supply. How has the illicit opioid supply, steeply escalating over the past decade, arisen to become the single greatest lethal driver of our overdose crisis today? Miron assigns no blame to the Mexican cartels responsible for greatly expanded “marketing” of heroin and now deadly fentanyl throughout the United States.
Rather, he offers the familiar view that a “crossover” took place from the licit to the illicit market because the criminal justice system and the medical profession tightened restrictions on opioid access. This narrative, though popular, is misleading; in fact, the rise of the illicit opioid market was underway even before efforts to limit prescribing intensified. Opioid prescribing may have increased the susceptibility of Americans to the opioid crisis, but legal efforts to control overprescribing did not initiate its effects.
Further, Miron trots out standard claims about the putative benefits to society of unrestricted opioid access regulated only by consumer choice in an abundant marketplace. No effort is made to address the question of whether the addicted truly exercise “choice” in their market behavior.
Nor does he address the question of what to do with users or potential users who are underage. Does no one under the “age of consent” require our protection? If so, have we not agreed to some system of “prohibition,” in principle? What of those who would nevertheless seek to “market” opioids to them?
Moreover, what of those who experience not a legal prohibition on their desired (and ceaselessly escalating) dosage, but rather a “marketplace” limitation, in that they cannot afford the full desired amount, multiple times a day? Are the opioids to be dispensed gratis by government, or would they be priced, and perhaps taxed?
And are we to place the feckless and trapped “citizens” under custodianship, and maintain them in their addicted state? Would society not require at least some restriction on the full exercise of their other rights, such as in employment, or voting, or driving, or gun ownership?
We see immediately that these necessary restrictions—prohibiting some use by some individuals at certain dosages—will occasion the persistence of an illegal “black market” in opioid supply, which will serve those whom the legal market declines to serve.
Yet allegedly this black market, the very forces currently operating with coercion and corruption and even violence, providing ever more dangerous (and desirable) opioid products at great profit, would somehow wither away in the presence of an authoritative marketplace scheme.
Experience teaches us that such does not happen. The real likelihood is that the opioid utopia Miron imagines will usher in the worst of future worlds: more prevalent and more frequent use, continued criminal justice concerns involving both the dispensation of the drugs and the consequent behavior of those addicted, and a staggering public health debacle of great economic and human cost.
His proposal is not an instance of the cure’s being worse than the disease, but of the cure being the disease—albeit in more virulent form.